Group health insurance typically covers pre-existing conditions, providing employees with access to necessary healthcare services.
Myth 1: Group Health Insurance Does Not Cover Pre-existing Conditions
Group Health Insurance does cover pre-existing conditions, contrary to the myth that it does not. This coverage ensures that individuals with existing health issues can still receive medical benefits under the group plan, providing essential support for their healthcare needs.
Explanation Of Pre-existing Condition Coverage In Group Plans
Group health insurance does cover pre-existing conditions within certain guidelines.Limitations And Waiting Periods
Coverage for pre-existing conditions may have limitations and waiting periods. Myth 1: Group Health Insurance Does Not Cover Pre-Existing Conditions Many believe group health insurance doesn’t cover pre-existing conditions, which is not entirely true. Group insurance does provide coverage for pre-existing conditions, though, with some restrictions and waiting periods. The coverage and limitations can vary from one plan to another.
Credit: http://www.simonandschuster.com
Myth 2: Employers Can Deny Coverage For Pre-existing Conditions
One of the common misconceptions about group health insurance is the belief that employers have the power to deny coverage for pre-existing conditions. This myth has caused confusion and worry among employees who may be dealing with ongoing health issues. However, the truth is that employees are protected by various legal provisions that prevent employers from denying coverage based on pre-existing conditions. Let’s take a closer look at the legal protections in place and the exceptions and responsibilities that employers have in relation to pre-existing conditions.
Legal Protections For Employees
Under the Health Insurance Portability and Accountability Act (HIPAA), employees have legal protections that ensure coverage for pre-existing conditions. HIPAA prohibits group health plans from imposing pre-existing condition exclusions (PCEs) on individuals who meet certain criteria. This means that if you have a pre-existing condition, your employer-sponsored group health insurance cannot deny you coverage or charge higher premiums than they do for employees without pre-existing conditions.
Additionally, The Affordable Care Act (ACA) expanded these legal protections further. ACA states that group health insurance plans, including those provided by employers, must cover essential health benefits, which include treatment for pre-existing conditions. This means that employers cannot discriminate against employees based on their medical history and must provide coverage for necessary medical treatment, regardless of pre-existing conditions.
Exceptions And Employer Responsibilities
While employers cannot outright deny coverage for pre-existing conditions, there are some exceptions and responsibilities that they have. For example, group health insurance plans may have a waiting period before providing coverage for pre-existing conditions. However, this waiting period is typically limited to a maximum of 12 months.
Employers are also required to provide employees with a Certificate of Creditable Coverage when they leave the company or experience a qualifying event that triggers a loss of coverage. This certificate serves as proof of previous coverage and helps individuals maintain continuous coverage even when switching jobs or insurance plans.
It’s important to note that while employers are legally obligated to provide coverage for pre-existing conditions, they may still have the ability to impose restrictions on coverage for treatments related to those conditions. This means that certain treatments or medications may have limitations or requirements for coverage, such as pre-authorization or specific networks of healthcare providers.
Overall, it’s crucial for employees to be aware of their legal protections when it comes to pre-existing conditions and group health insurance coverage. By understanding their rights and responsibilities, individuals can make informed decisions and ensure they receive the necessary healthcare they need.
Myth 3: Pre-existing Conditions Lead To Higher Premiums
Myth 3: Pre-Existing Conditions Lead to Higher Premiums
It’s a common misconception that individuals with pre-existing conditions will inevitably face higher premium rates in group health insurance plans. Let’s debunk this myth by delving into the factors influencing premiums in group health insurance.
Factors Influencing Premiums In Group Health Insurance
Group health insurance premiums are influenced by several factors, with pre-existing conditions being just one of them. Other factors include the age of the employees, the location of the business, and the level of coverage offered.
Community Rating Vs. Experience Rating
Group health insurance plans can be structured using either community rating or experience rating. Community rating sets premiums based on the average risk of the entire community, while experience rating adjusts premiums based on the claims history of the specific group. Understanding how these rating methods work is crucial in dispelling the myth that pre-existing conditions always lead to higher premiums.
Dispelling Common Misconceptions
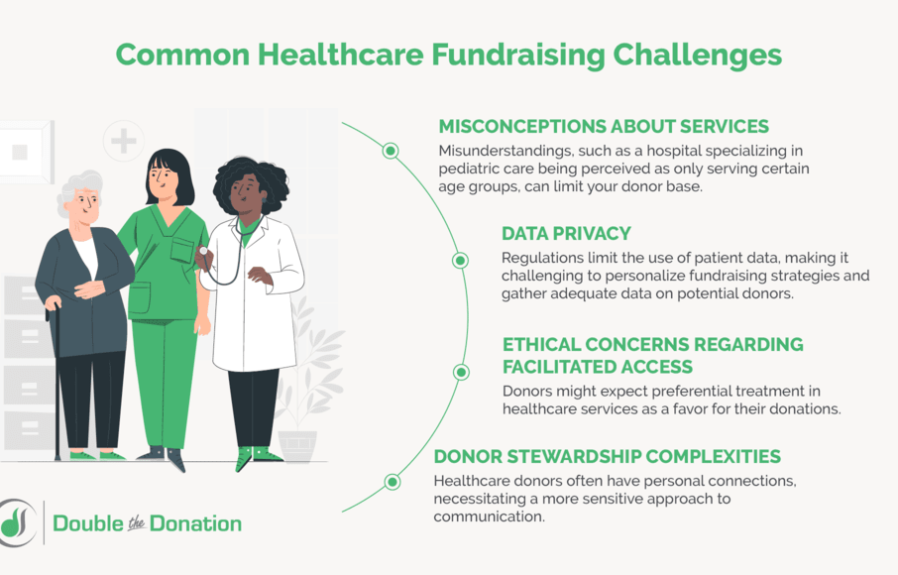
In the realm of group health insurance, there are several misconceptions surrounding coverage for pre-existing conditions. Let’s dispel these myths and gain a clearer understanding of how group health insurance addresses pre-existing conditions and the negotiation process for coverage.
How Group Health Insurance Addresses Pre-existing Conditions
The inclusion of coverage for pre-existing conditions in group health insurance plans is mandated by law. This provides individuals with pre-existing conditions the opportunity to obtain coverage without facing exclusions or higher premium rates. Group health insurance plans, being designed to cover a large number of employees or members, are better equipped to mitigate the risk associated with pre-existing conditions. Hence, they are more likely to offer comprehensive coverage for such conditions.
Negotiating Coverage For Pre-existing Conditions
When it comes to negotiating coverage for pre-existing conditions within a group health insurance plan, it’s important to understand the terms and conditions set by the insurer. Employers or group administrators can negotiate with insurance providers to tailor the coverage to the specific needs of the group. Displaying a thorough understanding of the group’s medical history and providing data on the health status of its members may aid in these negotiations. It’s crucial to leverage this information to ensure that the group health insurance plan adequately accommodates pre-existing conditions without imposing excessive restrictions or waiting periods.
Benefits Of Group Health Insurance For Pre-existing Conditions
Group health insurance provides coverage for pre-existing conditions, ensuring employees with existing health issues can receive necessary medical care without financial strain. This benefit promotes employee well-being and boosts morale within the workforce.
Group health insurance can be a game-changer for individuals with pre-existing conditions, providing them with a range of benefits that offer peace of mind and financial protection. By joining a group health insurance plan, individuals with pre-existing conditions gain access to comprehensive care, financial protection, and significant cost savings.
Access To Comprehensive Care
One significant benefit of group health insurance for individuals with pre-existing conditions is access to comprehensive care. Group health insurance plans typically offer a wide network of healthcare providers, including specialists who have experience dealing with various medical conditions.
With access to a diverse panel of doctors, individuals can receive specialized care and cutting-edge treatments for their pre-existing conditions. These healthcare providers have a deep understanding of the unique needs of individuals with ongoing health issues and can provide personalized treatment plans to manage and improve their health.
Moreover, group health insurance plans often cover a range of services, including diagnostic tests, medications, surgeries, and follow-up visits. This ensures that individuals with pre-existing conditions can receive the necessary care without the fear of being denied coverage or facing substantial out-of-pocket expenses.
Financial Protection And Cost Savings
Group health insurance also provides significant financial protection for individuals with pre-existing conditions. Under these plans, members can benefit from a wide range of cost-sharing mechanisms, including co-payments, co-insurance, and deductibles. This allows individuals to share the financial burden of healthcare expenses with the insurance company, minimizing the impact on their wallets.
Additionally, group health insurance plans often negotiate favorable rates with healthcare providers, which can lead to substantial cost savings. These negotiated rates can result in lower costs for medical services, such as consultations and procedures, making healthcare more affordable for individuals with pre-existing conditions.
Furthermore, group health insurance plans typically have out-of-pocket maximums, which limit the amount individuals have to spend on healthcare. Once this maximum is reached, the insurance company covers all additional expenses, providing individuals with financial relief and protection against excessive medical bills.
In conclusion, group health insurance offers numerous benefits to individuals with pre-existing conditions, including access to comprehensive care, financial protection, and significant cost savings. By joining a group health insurance plan, individuals can receive the necessary treatment for their pre-existing conditions without the fear of being denied coverage or facing exorbitant medical expenses.

Credit: http://www.thezebra.com
:max_bytes(150000):strip_icc()/predictive-analytics.asp-final-fc908743618a4f9093dfdd1fa6e9815a.png)
Credit: http://www.investopedia.com
Frequently Asked Questions For Does Group Health Insurance Cover Pre Existing Conditions
Does Group Health Insurance Cover Pre-existing Conditions?
Group health insurance may cover pre-existing conditions, but it depends on the specific policy. Some plans may have waiting periods before covering pre-existing conditions, while others may offer immediate coverage. It’s crucial to review the policy details to understand how pre-existing conditions are handled under the plan.
How Can I Find Out If My Pre-existing Condition Is Covered?
You can find out if your pre-existing condition is covered by reviewing the plan’s policy documents or contacting the insurance provider directly. Look for details on waiting periods, coverage limitations, and any specific conditions that may apply to pre-existing conditions.
It’s important to understand the coverage before enrolling in a plan.
What Are Common Pre-existing Conditions Covered By Group Health Insurance?
Group health insurance often covers common pre-existing conditions such as diabetes, hypertension, asthma, and allergies, among others. However, coverage may vary between plans, so it’s important to review the specific policy details to ensure that your pre-existing condition is included in the coverage.
Can I Be Denied Coverage For A Pre-existing Condition Under Group Health Insurance?
Under the Affordable Care Act (ACA), group health insurance cannot deny coverage or charge higher premiums based on pre-existing conditions. However, certain grandfathered or self-funded plans may have different rules. It’s essential to understand the regulations that govern coverage for pre-existing conditions under the specific plan.
Conclusion
Group health insurance can offer coverage for pre-existing conditions depending on the terms and conditions set by the insurance provider. It is important for individuals to thoroughly understand the policy and its limitations, as well as any waiting periods or exclusions that may apply.
By researching and comparing different plans, individuals can find the right group health insurance that caters to their specific needs and provides coverage for pre-existing conditions.


Leave a comment