Yes, insurance can cover therapy to varying degrees depending on the type of insurance plan and the specific therapy being sought. Insurance coverage for therapy is contingent upon factors such as the individual’s policy, provider network, diagnosis, and treatment goals.
Therapy services may fall under mental health benefits, which can include coverage for individual therapy, group therapy, family therapy, or couples therapy. To determine if therapy is covered by insurance, individuals should review their policy, consult with their insurance provider, and inquire about any necessary pre-authorization or referral requirements.
It is important to note that coverage can differ widely between insurance companies and plans, so it is advised to thoroughly understand the terms and limits of coverage before beginning therapy.
Types Of Therapy
Cognitive Behavioral Therapy (cbt)
Cognitive Behavioral Therapy (CBT) is a type of therapy that focuses on changing negative thought patterns and behaviors.
Psychodynamic Therapy
Psychodynamic Therapy delves into unconscious thoughts and past experiences to understand present emotions and behaviors.
Family Therapy
Family Therapy involves sessions with family members to address and resolve conflicts and improve communication.
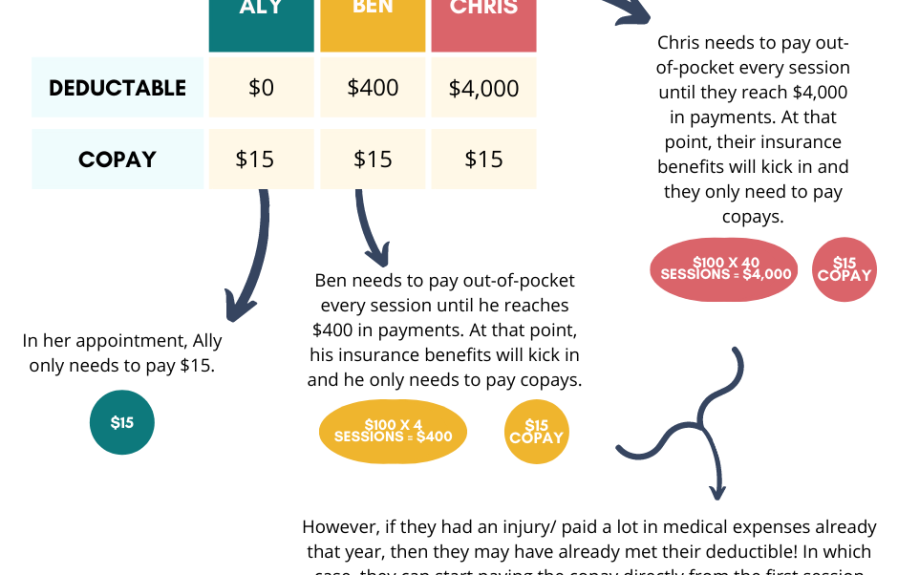
Credit: http://www.behaviorfrontiers.com
Understanding Insurance Coverage
When seeking therapy, one of the most common questions is whether insurance covers the cost. Understanding insurance coverage for therapy can be a complex topic, and it’s important to have a clear understanding of the different types of insurance plans and whether your therapist is considered in-network or out-of-network. In this article, we will break down these key elements to help you navigate your insurance coverage for therapy.
Types Of Insurance Plans
Insurance plans can vary greatly in terms of coverage and benefits. It’s essential to be aware of the type of insurance plan you have when considering therapy. Here are some common types of insurance plans:
- Health Maintenance Organization (HMO): HMO plans usually require you to choose a primary care physician (PCP) who will coordinate your healthcare needs. To see a therapist, you typically need a referral from your PCP.
- Preferred Provider Organization (PPO): PPO plans offer greater flexibility when choosing a healthcare provider. You have the option to see therapists both within and outside of the network, although there may be different levels of coverage for in-network and out-of-network providers.
- Point of Service (POS): POS plans combine elements of HMO and PPO plans. You may need a referral to see a therapist and have the option to see out-of-network providers, but with higher out-of-pocket costs.
In-network Vs. Out-of-network Providers
When it comes to insurance coverage, it’s essential to understand whether your therapist is considered in-network or out-of-network. Here’s what you need to know:
| In-Network Providers | Out-of-Network Providers |
|---|---|
| In-network providers have an agreement with your insurance company, which means they have agreed upon rates and have met certain quality criteria. With an in-network therapist, your insurance will typically cover a portion of the therapy costs, and you’ll be responsible for any applicable copayments, coinsurance, or deductibles. | If you choose an out-of-network therapist, they do not have a contract with your insurance company. This means you may have to pay the full cost of therapy upfront and then seek reimbursement from your insurance company. It’s essential to understand your out-of-network benefits and any potential limitations or restrictions. |
Understanding the ins and outs of insurance coverage for therapy can save you from unexpected expenses and help you make informed decisions. Take the time to review your insurance plan and consult with your insurance provider or human resources department to clarify any uncertainties about your coverage. With a clear understanding of your insurance coverage, you can make the best choices for your mental health and well-being.
Factors Affecting Coverage
Insurance coverage for therapy depends on several factors, including the type of insurance plan, the specific therapy needed, and whether the therapist is in-network or out-of-network. Additionally, the individual policy terms and deductibles play a crucial role in determining coverage eligibility.
Factors Affecting Coverage Understanding the factors that affect therapy coverage by insurance can play a significant role in accessing the treatment you need. Insurance Company Policies, Diagnosis Requirements are two important factors that determine whether therapy sessions will be covered. Knowing how these elements influence coverage can help you navigate the insurance process more effectively.Insurance Company Policies
The coverage for therapy is largely determined by the specific policies of your insurance company. Different insurance providers have varying levels of coverage for mental health services, including therapy. It’s essential to review your policy to understand the specifics of your coverage and any limitations that may apply. Some insurance plans may limit the number of sessions covered, while others may require pre-authorization or have specific network providers.Diagnosis Requirements
Many insurance plans require a diagnosis of a mental health disorder to cover therapy sessions. This means that the therapist must provide a formal diagnosis that meets the criteria outlined by the insurance company. It’s important to ensure that your therapist is able to provide the necessary documentation to support the diagnosis required for coverage. The specific diagnoses that are eligible for coverage may vary between insurance plans, so it’s crucial to verify the requirements with your insurance provider. Understanding these factors is essential for navigating the complexities of insurance coverage for therapy. By being aware of your insurance company’s policies and the diagnosis requirements, you can better advocate for yourself and work with your therapist to ensure that you can access the treatment you need. If you want to know more about the coverage of therapy by insurance, you can reach out to a mental health professional or refer to the official website of your insurance provider for specific details.
Credit: http://www.autismlearningpartners.com
Checking Coverage
When seeking therapy, one crucial aspect to consider is whether your insurance provides coverage. Understanding your insurance policy and what it encompasses can help mitigate the cost of therapy sessions. Here’s how you can verify whether your insurance covers therapy.
Contacting Your Insurance Provider
Contact your insurance provider to ascertain the details of your coverage for therapy sessions. Obtain the customer service contact information from your insurance card or their website. When you get in touch with them, be prepared to provide your policy number and personal details.
Reviewing Your Policy
Review your insurance policy to determine the specifics of your coverage for mental health services. Pay attention to mental health, behavioral health, or counseling to identify any indications of therapy coverage. Look for any restrictions, limitations, or copay requirements.
Alternatives To Insurance Coverage
Therapy costs can add up, and insurance coverage for such services may not always be comprehensive. However, there are alternatives to consider, such as employer assistance programs, sliding scale fees, or health savings accounts, which can help individuals access therapy without solely relying on insurance coverage.
While insurance coverage can be beneficial, it may not always be available or affordable for everyone seeking therapy. Fortunately, there are alternatives that can help individuals access the support they need without relying on insurance. Here are two common alternatives:
Sliding Scale Fees
Sliding scale fees are a payment option offered by many therapists and counseling centers. It provides individuals with a flexible pricing structure based on their income level, ensuring that therapy remains accessible to all. With sliding scale fees, the cost of therapy is adjusted according to the individual’s financial situation. For those with lower incomes, the fees are reduced, making therapy more affordable.
Sliding scale fees can be an excellent option for those without insurance or with limited coverage. This is particularly beneficial for individuals facing financial constraints but still seeking the support and guidance of therapy. It ensures that no one is denied therapy solely based on their inability to pay the full fee.
Nonprofit Organizations
Another alternative to insurance coverage for therapy is seeking assistance from nonprofit organizations. Many nonprofits offer mental health services and counseling at reduced costs or even for free. These organizations are dedicated to providing support and resources to those in need, regardless of their insurance status or financial constraints.
Nonprofit organizations often have a mission to make therapy and mental health support accessible to all individuals. They may rely on grants, donations, and volunteers to offer their services at little to no cost. If you are unable to afford therapy through insurance or private practice, reaching out to nonprofit organizations can be a viable option.
In summary, when insurance coverage for therapy is not available or affordable, there are alternatives that can help individuals access the support they need. Sliding scale fees and nonprofit organizations offer flexible payment options and reduced-cost or free counseling services. These alternatives ensure that therapy remains accessible to everyone, regardless of their financial situation or insurance coverage.

Credit: blog.zencare.co
Tips For Maximizing Insurance Benefits
Proper documentation and utilizing teletherapy services can help you make the most of your insurance coverage for therapy.
Proper Documentation
Keep detailed records of your therapy sessions and progress to submit to your insurance provider.
Record the dates, duration, and outcomes of each session for easy access.
- Include notes on your symptoms and how therapy is helping you.
- Ensure your therapist fills out any required forms accurately.
Utilizing Teletherapy Services
Maximize your insurance benefits by taking advantage of teletherapy services when available.
Choose a provider who offers secure and HIPAA-compliant online therapy sessions.
- Confirm that your insurance covers teletherapy sessions.
- Schedule appointments that fit your needs and insurance coverage.
Frequently Asked Questions On Does Insurance Cover Therapy
Can Insurance Cover Therapy Costs?
Yes, many insurance plans provide coverage for therapy, including counseling and psychiatric services. However, coverage varies depending on your specific insurance plan and the type of therapy you need. It’s important to check with your insurance provider to understand your coverage and any potential limitations.
What Types Of Therapy May Insurance Cover?
Insurance providers generally cover a range of therapy options, including individual counseling, group therapy, family therapy, and psychiatric services. The specific types of therapy covered can vary based on your insurance plan and the nature of the therapy needed. Review your policy or speak to your insurance provider for clarity.
How Can I Find Out If My Insurance Covers Therapy?
To determine if your insurance covers therapy, contact your insurance provider directly or review your policy details. Your insurance company can provide specific information about the types of therapy covered, any limitations or requirements, and how to go about utilizing your coverage for therapy services.
What If My Insurance Doesn’t Cover Therapy?
If your insurance doesn’t cover therapy or provides limited coverage, there are still options available. You can inquire about sliding scale fees with therapists, seek out community resources, or explore alternative coverage options. It’s important to prioritize your mental health and explore all available avenues for accessing therapy.
Conclusion
Insurance coverage for therapy can vary depending on your specific policy and provider. It’s crucial to carefully review your plan and consult with your insurance company to understand the extent of coverage for mental health services. While some policies offer comprehensive coverage, others may have limitations or require pre-authorization.
Remember to prioritize your mental well-being and explore alternative options if therapy coverage is limited. Don’t hesitate to reach out to professional therapists and financial advisors for guidance.


Leave a comment